- Lakeside Commons, 990 Hammond Drive, Suite 325, Atlanta, GA 30328
- Tel: (404) 256-3720

A century ago, the only way to make a definite diagnosis for many neurological disorders was to perform an autopsy after someone had died. However today, with new instruments and techniques, along with other medical advances, we now have powerful and accurate tools to better diagnose disease.
Perhaps the most significant changes during the past ten years have occurred in genetic testing and diagnostic imaging. Much has been learned from sequencing the human genome (the complete set of a person’s genes) and developing new technologies that detect genetic mutations. Improved imaging techniques provide healthcare providers high-resolution images to view the structure of the brain. Specialized imaging methods can visualize changes in brain activity or the amounts of particular brain chemicals. Scientists continue to improve these methods to provide more detailed diagnostic information.
Researchers and healthcare providers use a variety of diagnostic imaging techniques and chemical and metabolic tests to detect, manage, and treat neurological disease. Many tests can be performed in a doctor’s office or at an outpatient testing facility, with little if any risk to the person. Some procedures are performed in specialized settings to determine specific disorders or abnormalities. Depending on the type of test, results may be immediate or may take time to process.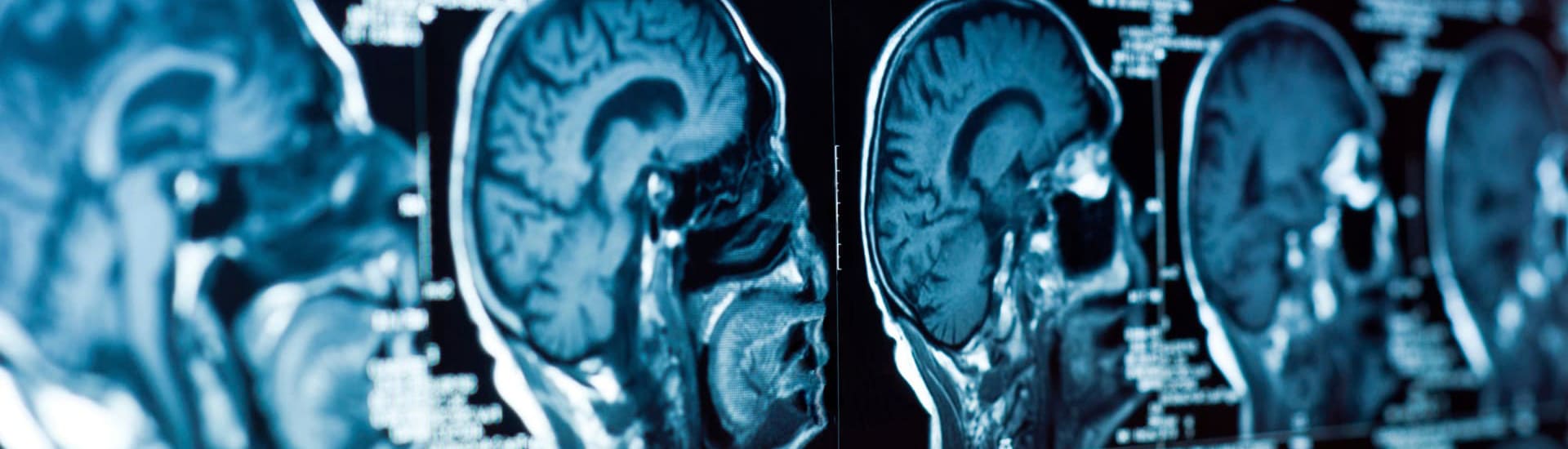
Brain scans include several types of imaging techniques used to diagnose tumors, blood vessel malformations, stroke, injuries, abnormal brain development, and hemorrhage in the brain. Types of brain scans include computed tomography (CT), magnetic resonance imaging (MRI), and single proton emission (SPECT) scans.
CT scanning takes about 20 minutes and is usually done at an outpatient imaging center or in a hospital. The person lies on a special table that slides into a narrow, doughnut-shaped chamber. A sound system built into the chamber allows the person to communicate with the physician or technician. X-rays (ionizing radiation) are passed through the body at various angles and are detected by a computerized scanner. The data is processed and displayed as cross-sectional images, or “slices,” of the internal structure of the body or organ. Occasionally a light sedative may be given if the person is unable to lie still and pillows may be used to support and stabilize the head and body.
If a contrast dye is injected into a vein, the individual being scanned may feel a warm or cool sensation as the dye circulates through the bloodstream or may experience a slight metallic taste. CT scans are particularly useful in people who are unable to undergo MRI. Because CT uses X-rays, pregnant women should avoid the test because of potential harm to the fetus.
An MRI scanner consists of a tube surrounded by a very large cylindrical magnet. These scanners create a magnetic field around the body that’s strong enough to temporarily realign water molecules in the tissues. Radio waves are then passed through the body to detect the shifting of molecules back to a random alignment. A computer then reconstructs a three-dimensional picture or a two-dimensional “slice” of the tissue being scanned. MRI can distinguish between bone, soft tissues, and fluid-filled spaces because of differences in water content and tissue properties. The individual lies on a special table that slides into the tube and will be asked to remove jewelry, eyeglasses, removable dental work, clothing with metal and other items that might interfere with the magnetic imaging. The person may hear grating or knocking noises when the magnetic field direction is flipped. Earphones or earplugs can help block out the sounds. For brain MRI scans, a detector is placed over the head.
Due to the incredibly strong magnetic field generated by an MRI, people with implanted medical devices such as a pacemaker or infusion device generally should not have MRIs. In certain circumstances facilities may have equipment to temporarily stop and reset the implanted device’s programming in order to allow MRI.
Unlike CT scanning, MRI does not use ionizing radiation to produce images. The test is painless and risk-free, although persons who are obese or claustrophobic may find it somewhat uncomfortable. Depending on the part(s) of the body to be scanned, MRI can take up to an hour to complete. Some centers use open MRI machines that do not completely surround the person being tested and are less confining. However, open MRI does not currently provide the same picture quality as standard MRI and some tests may not be available using this equipment.
Because people must remain still during the MRI, children may need to be sedated in order to be scanned. If intravenous contrast is required, people may first need a blood test to check kidney function because the contrast agent, called gadolinium, can increase the risk of a rare disease in people with advanced kidney disease.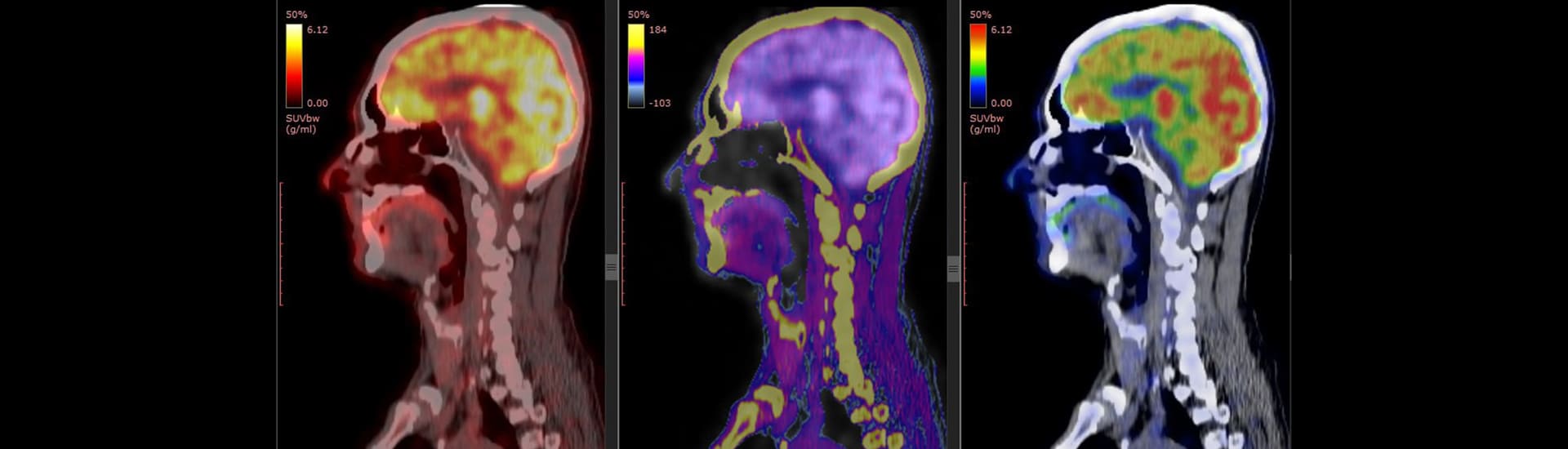

CSF analysis involves the removal of a small amount of fluid that surround the brain and spinal cord. It is commonly referred as a lumbar puncture or spinal tap. The fluid is tested to detect evidence of brain, hemorrhage, infection, multiple sclerosis, metabolic diseases, or other neurological diseases. The pressure inside the skull can be measured to detect conditions in the brain (e.g. benign intracranial hypertension).
During the lumbar puncture the person will either lie on one side, with knees close to the chest, or lean forward while sitting on a table or bed. The patient’s back will be cleaned and injected with a local anesthetic. The injection may cause a slight stinging sensation. Once the anesthetic has taken effect, a special needle is inserted between the vertebrae into the spinal sac and a small amount of fluid (usually about three teaspoons) is withdrawn for testing. Most people will only feel a sensation of pressure as the needle is inserted. Generally, people are asked to lie flat for an hour or two to reduce the after-effect of headache. There is a small risk of nerve root injury or infection from a lumbar puncture. The procedure takes about 45 minutes.
If the results on any part of the neurological examination are abnormal, laboratory studies may be ordered to help make a diagnosis. Laboratory screening tests of blood, urine, or other body fluids may help diagnose disease, understand disease severity, and monitor levels of therapeutic drugs. Certain tests provide general information, while others are used to identify specific health concerns. For example, blood tests can provide evidence for infections, toxins, clotting disorders, or antibodies that signal the presence of an autoimmune disease. Genetic testing of DNA extracted from cells in the blood or salvia can be used to diagnose hereditary disorders.
Analysis of the fluid that surrounds the brain and spinal cord can detect meningitis, encephalitis, acute and chronic inflammation, viral infections, multiple sclerosis, and certain neurodegenerative disorders. Chemical and metabolic testing of the blood can indicate some muscle disorders, protein or fat-related disorders that affect the brain and inborn errors of metabolism. Blood tests can monitor levels of therapeutic drugs used to treat epilepsy and other neurological disorders. Analyzing urine samples can reveal toxins, abnormal metabolic substances, proteins that cause disease, or signs of certain infections.
These tests may include one or more of the following:Reference: The National Institute of Neurological Disorders and Stroke